Blood Tests for Depression
Could a simple blood test detect the efficacy of antidepressants on those with depression? A new study suggests it’s a possibility.
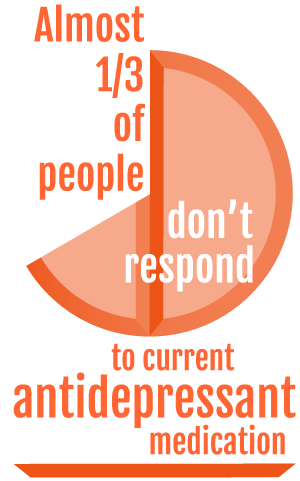
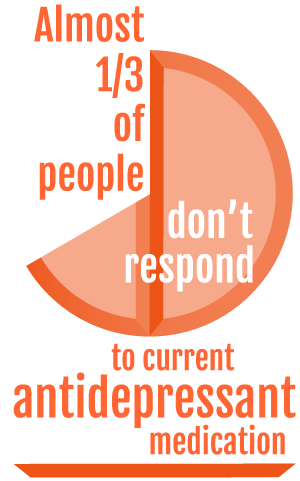
It has long been known that first-line anti-depressants are not effective treatment options for everyone. While some people may find success with their first treatment option and others may have to work through a few options before settling on a medication that works, for almost a third of people current antidepressant medication does not work. This is frustrating, not least because many antidepressants can have unpleasant side effects, which the patient then has to deal with without any relief from the initial issue of depression.
This could change.
 For the first time a study has found reliable links between biomarkers in those who live with depression and their likelihood of response to anti-depressants.
For the first time a study has found reliable links between biomarkers in those who live with depression and their likelihood of response to anti-depressants.
A paper, published in the International Journal of Neuropsychopharmacology, has found there are high levels of inflammation evident in those individuals resistant to traditional antidepressant medication. This could mean that something as simple as a blood test could help determine the likelihood of an individual responding positively to traditional antidepressants.
The findings suggest that the identification of biomarkers in predicting treatment response could not only significantly reduce the social and economic burden of depression in the community but importantly, improve the quality of life of patients.
Biomarker: a naturally occurring molecule, gene, or characteristic by which a particular pathological or physiological process, disease, etc. can be identified.
Depression is one of the most common mental illnesses in the world, with around 1 million people in Australia living with it. As anyone who has ever had to live with depression can attest, the process of finding an antidepressant that works for you can be long and unpleasant.
There are the side effects, which can include insomnia, headaches, nausea and weight fluctuation, as well as the chance that one or more antidepressants may not work effectively. Knowing in advance whether or not you are biologically predisposed to respond favourably to medication is a huge step forward.
One of the most interesting findings of the trial was the inflammatory biomarkers that suggest a pre-eversion to traditional medication are also triggered by events such as childhood trauma. This in itself is associated with poor antidepressant response. It was also found that these biomarkersappear to be genetically acquired, meaning that a predisposition to antidepressant resistance could be passed down through families.
While there is much to applaud in the research, it is important to note the study is still in its infancy and has yet to undergo clinical trials.
This will help hone the accuracy of the research and develop ways of applying it to real-life situations.
The study is also solely based on a prediction of response to antidepressants in general and is not specific to one type of medication. Therefore, the research cannot be used to guide the choice of antidepressant medication but to identify those individuals who may benefit from adjuvant therapies.
For the uninitiated there are six or seven main classes of antidepressant medications that all work in slightly different ways. The two primarily prescribed are either Selective Serotonin Re-uptake Inhibitors (SSRIs) or Serotonin and Noradrenaline Reuptake Inhibitors (SNRIs). If a doctor prescribes an SSRI such as Lexapro, Prozac or Zoloft and it is not helping to relieve depressive symptoms they will often try other antidepressants such as SNRIs like Effexor and Remeron.
Medical practitioners may continue to try different types of antidepressants if the two common medications do not work. Other less often prescribed types of medication include RIMAs, TCAs, NaSSAs, NARIs and (rarely) MAOIs.
Finding the correct fit of medication for each individual can be a long process with each medication requiring a period of adjustment. While this study has found markers that suggest when medication will not be effective,it has not found a way of discovered which particular medications will be most effective for those who find first-line antidepressants ineffective. That is a question for future studies.
Comprehensive studies have yet to be undertaken, however, research indicates that successful treatment of depression reduces the levels of these biomarkers in the blood, suggesting their presence is directly related to the onset of depression.
In terms of those who respond poorly or fail to respond at all to first-line antidepressants, this research could mean alternative treatment strategies, such as cognitive behaviour therapy (CBT) and psychotherapy, are deployed early in the course of treatment to achieve the best outcomes.
While there is still a way to go before a blood test detects how effective a medication is for an individual, the study indicates a positive push forward for further advancements in mental healthcare.
If you are interested in reading further the full study can be found here: http://ijnp.oxfordjournals.org/content/early/2016/06/02/ijnp.pyw045
Jean Roxon
Newsletter
Stay up to date
Sign up to our Mind Reader newsletter for monthly mental health news, information and updates.